|
|
|
| Combined Non-surgical And Surgical Endodontic Therapy In The Treatment Of Dens In Dente Type Iii With Mta Retroseal- A Case Report |
Ridhi Garg 1 , Ankit Singhal 2 , Rajnish Agarwal 3 , Renu Agarwal 4
1 Senior Lecturer, Department of Endodontics - Dr B.R. Ambedkar Dental College,Patna,Bihar,India.
2 Senior Lecturer, Department of Orthodontics - Dr B.R. Ambedkar Dental College,Patna,Bihar,India.
3 Senior Lecturer, Department of Prosthodontics - Surendra Dental College & Research Institute, Sriganganagar, Rajasthan
4 Senior Lecturer, Department of Endodontics - Surendra Dental College & Research Institute, Sriganganagar, Rajasthan
|
| Address For Correspondence |
Dr. Ridhi Garg, Senior Lecturer, Dept. of Endodontics,
Dr B.R. Ambedkar Institute Of Dental
Sciences & Hospital, Hariomnagar,
New Bailey Road(West Of Canal) Patna, Bihar. |
| Abstract |
| Dens invaginatus is a maldevelopment of the dental germ which occurs as a result of the invagination of the enamel organ. Dens invaginatus requires early diagnosis and treatment, as it may result in radicular and periapical pathosis. Treatment may vary from case to case. The successful management of dens invaginatus depends mainly on the ability to gain access to and disinfect the root canal system in light of its complex and variable presentation and unpredictable morphology. This study describes a clinical case of type III dens invaginatus with an extensive periradicular lesion and open apex treated successfully. |
|
| Keywords |
| dens in dente, dens invaginatus, pulp necrosis, periapical pathology, MTA retroseal. |
|
| Full Text |
Introduction
Dens invaginatus is a variation in the development of tooth which is thought to occur when there is infolding of the enamel organ during the bell stage before beginning of calcification.[1] The term synonymous with this malformation are telescopic tooth, dilated odontoma, dens in dente, dilated composite odontoma and tooth inclusion.[2] It’s a rare developmental malformation with frequency of 0.04-10%.The teeth most commonly affected are maxillary lateral incisor with a prevalence of 0.25%-5% followed by central incisors, premolars, canines and molars.[3] Bilateral occurrence is not uncommon and occurs in 43% of all cases.
Numerous mechanisms have been proposed as a cause of this phenomenon including local delay in enamel formation, infolding of the enamel organ with in dental pulp and local external influences on tooth germ. The etiology is still not entirely known.
Ohler has classified dens invaginatus in three types depending on its extent in crown (type I), root (type II) and up to apex (type III)[4]. Clinically the crown of this tooth can be of normal morphology but can also have unusual forms. A deep palatal groove can be the first sign indicative of dens invaginatus. In this type of developmental anomaly there may be direct communication between the pulp and the oral cavity. When this is the case, microorganisms from saliva infect the pulp and necrosis may lead to the formation of an apical lesion. Many investigators have reported the occurrence of pulpal and periapical pathosis related to dental invaginations, which suggest that apical pathosis from pulpal death is a common occurrence related to caries or defects within invagination.[2]
Several treatments of pathosis associated with dens invaginatus has been suggested which include endodontic therapy, endodontic surgery, combined treatment or extraction. This article presents a case report of a type III dens invaginatus with open apex and a large periradicular pathology which is managed successfully by combined non surgical and surgical endodontic therapy with MTA retroseal.
Case Report
A-24–year male patient reported with a complaint of swelling on left side of face. During an extraoral examination a slight facial asymmetry was observed with edema on middle third of left side of face including maxillary region, nostril, and upper lip. Intraoral examination revealed swelling in vestibular region of maxillary left lateral incisor (Tooth no 9) and an anatomic anomaly of the lingual surface of the tooth in the form of an accessory cusp. The tooth did not respond to pulp vitality tests suggesting pulp necrosis. The radiographic examination revealed the presence of dens invaginatus type III with large periapical radiolucency in the involved tooth. Apex of the tooth was wide open indicative of blunderbuss canal (Figure - 1). Endodontic treatment followed by surgical enucleation of the lesion and retrograde filling of the root to seal the apex was therefore planned for this tooth.
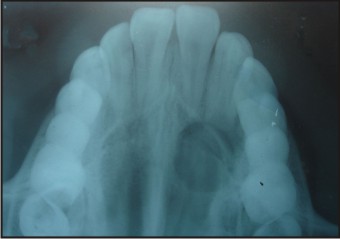 | Figure-1: Pre Operative Occlusal Radiograph Showing Left Maxillary Lateral Incisor With Dense In Dente Type Iii Having Large Periapical Radiolucency And Open Apex.
 |
For endodontic treatment following isolation of tooth with rubber dam, pulp chamber was opened. As access opening was made, a normal shaped root canal and adjacent very narrow rudimentary canals were found. There did not appear to be any connection between central root canal and the rudimentary canals. As the canals were opened pus drainage from the canals occurred. Working lengths of the canals were then established and the chemo-mechanical preparation was carried out using manual coronal apical instrumentation technique with manual stainless steel k- file. (Denstply, Ballaigues, Switzerland). Canals were flushed copiously with 2.5% sodium hypochlorite. The final irrigation was done with 17% EDTA, followed by 1% sodium hypochlorite. Sterile paper points were used to dry the canals and a calcium hydroxide paste was placed. The coronal access was sealed with GIC (GC 2,GC Corporation, Tokyo, japan). Patient was recalled for the medication change every week for a month. However intracanal exudates were present suggesting resistant infection in apical region. Periapical surgery was therefore planned as a complimentary approach. Prior to surgery root canal obturation was carried out by gutta percha using lateral condensation technique (Figure - 2). The surgical intervention consisted of apical curettage, root end resection, root end preparation with ultrasonic tips and retrofilling. A vestibular flap was raised, granulation tissue was removed, root end prepared and retrofilling with proroot MTA was done (Figure - 3).
 | Figure-2: Radiograph Showing Central Canal And Rudimentary Canals.
 |
 | Figure-3: Radiograph Showing Obturated Root Canals And Mta Retroseal.
 |
At 1 year follow up examination, the patient was asymptomatic and radiographic evidence of satisfactory healing was confirmed by decrease in size of radiolucency (Figure - 4).
 | Figure-4: One Year Follow Up Radiograph Showing Healing.
 |
Discussion
Dens invaginatus is a tooth abnormality of clinical significance due to the possibility for the pulp to be affected which may further lead to radicular and periapical pathosis. In dens invaginatus the invaginated area is separated from the pulpal tissue with a thin layer of dentin thus a carious lesion can easily reach the pulp chamber. Therefore pulpitis and pulp necrosis are frequently associated with this anamoly.[3] Many investigators have reported the occurrence of pulpal and periapical pathosis related to dental invaginations, which suggests that apical pathosis from pulpal death is a common occurrence related to caries or defects with in invagination. In this case tooth no 9 was clinically healthy, caries free and without history of trauma. Thus the etiology of the chronic periapical lesion was probably pulp necrosis caused by the passage of bacteria through the invagination defect, creating direct communication between the oral cavity and the pulp chamber.
The treatment options for an invaginated tooth include prevention treatment by sealing or filling in the invagination, endodontic treatment, apical endodontic surgery, intentional reimplantation and exodontics.[5] In the current case radiograph revealed invagination on maxillary lateral incisor extending from crown to the apex of the root (Ohler’s type III), the involved tooth was also associated with a large periapical pathosis and wide open apex. So a combination of orthograde endodontic treatment and endodontic surgery was planned for its treatment.
Root canal treatment is based primarily on the removal of microbial infection from the complex root canal system. Since the pulp of this tooth was necrotic as it did not respond to pulp vitality tests, orthograde endodontic treatment was done to clean and disinfect the root canals and to seal them permanently to avoid further infection. During endodontic treatment the different root canals were instrumented separately as there did not seem to be any communication between the different root canals. Unnecessary merging the canals would lead to tooth weakening because of more dentin removal. So merging of the canals was deemed unnecessary. During chemo-mechanical preparation, the use of rotary instrument is not recommended because of the presence of an enamel lining in the lumen of the invagination and an inconsistent shape of the canal which may increase the likelihood of instrument fracture. Therefore canals were instrumented using hand files. Irrigants aid in reducing the microflora of infected canals and if a tissue solvent is used, can help to dissolve the necrotic tissue. Therefore 2.5% hypochlorite was used as an irrigating solution because of its tissue dissolving property.[6] However studies have revealed that instrumentation and irrigation with sodium hypochlorite alone is not sufficient to leave the root canal free from cultivable bacteria and their endotoxins. Thus in order to compliment the actions of the instruments and irrigating solutions, the use of intracanal medicament is recommended. Calcium hydroxide has commonly been used, which has antimicrobial activity and can inactivate endotoxins[7].
Considering the need for the complete removal of all the irritants from the root canal system, the use of an irrigating solution associated with successive change of intracanal medication based on calcium hydroxide was essential for the success of the treatment.
Surgical intervention was done for two reasons. First the apex of the tooth was wide open so a retrograde sealing of the apex with a root end filling material was required. The purpose of root end filling is to establish an impermeable seal of all the apical avenues of the root canal system and prevent the percolation of bacteria or their products between the root canal systems and periradicular tissues. Second reason for periradicular surgery was the large size of the lesion as suggested by the large periapical radiolucency in the radiographs. Literature suggests when apical radiolucency is very large (diameter >20mm or cross sectional ares >200mm2), surgical removal may be the best option[8]. According to Pai et al ,the complex anatomy of dens invaginatus makes it difficult and usually complicates the conservative endodontic treatment, especially when large apical lesion exists.[9]
In the present case because of the large size of the lesion, radiographic appearance suggesting lesion being cystic and long standing nature of the infection surgical intervention was done. MTA was chosen as a retrograde filling material because of its better physical and chemical properties as a retrograde filling material.[10]
Therefore orthograde endodontic treatment was done to clean, disinfect and to seal the root canals. The surgery was done to debride the periapical lesion and to provide an additional retrograde seal to the root canals which may remain a source of irritation.
Conclusion
Because of complication presented by dens invaginatus type III, open apex of the root and a large periapical lesion combined nonsurgical and surgical endodontic therapy was indicated in this case. Follow up radiograph over 1 year showed evidence of healing.
References
1. M.Hulsmann, Dens invaginatus: etiology, classification, prevalence, diagnosis and treatment considerations.Int Endod J 1997; 30, 79-90.
2. Reddy YP, Karpagavinayagam K, Subbarao CV.Management of dens invaginatus diagnosed by spiral computed tomography.J Endod 2008; 34, 1138-42.
3. Mupparapu M, Singer SR.A rare presentation of dens invaginatus in a mandibular lateral incisor occurring concurrently with bilateral maxillary dens invaginatus. Case report and review of literature. Australian dental journal 2004; 49, 90-3.
4. F.A Oehlers.Dens invaginatus, 1.Variation of the invagination process and associated anterior crown forms.Oral Surg Oral Med Oral Pathol 1957; 10, 1204-18.
5. Canger EM,Kayipmaz S, Celenk P. Bilateral dens invaginatus in the mandibular premolar region .Ind J Dent Res 2009; 20 (2), 238-40.
6. Martinho FC, Gomes BPFA.Quatification of endotoxins and cultivable bacteria in root canal infection before and after chemo-mechanical preparation with 2.5%sodium hypochlorite.J Endod 2008; 34, 268-72.
7. Mohhammed Z,Dummer PMH .Properties and application of calcium hydroxide in endodontics and dental traumatology.Int Endod J 2011; 44(8), 697-730.
8. Natkin E, Oswald RJ, Carnes LI. The relationship of lesion size to diagnosis, incidence,and treatment of periapical cysts and granulomas. Oral Surg Oral Med Oral Pathol 1984; 57, 82–94.
9. Pai SF,Yang SF,Lin LM.Nonsurgical endodontic treatment of dens invaginatus with large periradicular lesion.A case report .J Endod 2004; 30 (8), 597-600.
10. Shabahang S, Torabinejad M.Treatment of teeth with open apices using mineral trioxide aggregate .Pract Periodontics Aesthet Dent 2000; 12, 315-20. |
|
|
|
|
|
|